Astounding: Takes You Inside Cutting-Edge Robotic Procedures in a Shocking Documentary!
Planet TV Studios reveals an exposé regarding Dr. Brandon Gough's Revolutionary Surgical Methods within "New Frontiers" – Screening March, 2024 on Countrywide TV plus Instant Access.
BOCA RATON, FL, UNITED STATES, March 1, 2024 /ReportWire.org -- Planet TV Studios with pride showcases its latest documentary installment, "New Frontiers," spotlighting the cutting-edge triumphs by Gough Surgical, PLLC. This series provides insight into the paradigm-shifting developments pioneered by Dr. Brandon Gough, M.D., an eminent musculoskeletal surgeon with expertise in cutting-edge microinvasive techniques in addition to robot-assisted hip and knee arthroplasty.
"New Frontiers" constitutes an engaging journey thoughtfully assembled to showcase avant-garde groups directing the advancement of global medical care. Be sure to view the sequential documentary releases broadcast during the mid-2024 period through countrywide TV channels, Bloomberg TV, plus streamable on-demand on platforms including Amazon’s streaming service, Google Play, Roku, and further digital outlets.
Planet TV Studios is honored to host Gina Grad returning as the presenter. Gina is celebrated as an established author, podcast emcee, and voice of the airwaves based in Los Angeles, California. She previously served as serving as both co-host and news anchor on the Adam Carolla Show, a podcast famous for its Guinness World Record in episode downloads. Gina has provided anchoring for KFI 640 AM and directed morning programming on 100.3 FM. She is now leading "The Bryan and Gina Show, The Official Podcast of LA Magazine." In addition to her broadcasting career, she authored "My Extra Mom," a picture book crafted to help children and non-biological parents in overcoming the obstacles of integrating families.
Dr. Brandon Gough, M.D., emerges as a notably acclaimed orthopedic surgeon, board certified and renowned for his expertise in procedures for hip and knee reconstruction through the region of Phoenix, Arizona. Employing state-of-the-art robotic technology alongside micro-invasive and muscle-sparing surgical methods, Dr. Gough endeavors to foster prompt returns to a swift return to normal activities post-surgery. His emphasis on preserving soft tissue accelerates recuperation while reducing hospital time and, at times, allows for outpatient total joint replacement surgeries. He is celebrated as an international pioneer in the Direct Superior Approach and muscle-sparing robotic-assisted methods.
Recognizing education as fundamental, Dr. Gough leverages continual learning to provide first-rate patient care in Orthopedic Medicine. Following his college education at Spring Hill College from Mobile, Alabama, he obtained his medical degree from Creighton University School of Medicine situated in Omaha, Nebraska. Dr. Gough cultivated his expertise through his residency and internship in General Orthopedics at the University of Kansas, School of Medicine from Wichita, KS, receiving accolades as the Resident Teacher of the Year. He undertook further specialized training through a fellowship in Lower Extremity Adult Reconstruction at the Arizona Institute of Bone and Joint Disorders.
Being board-certified by the American Board of Orthopedic Surgeons and actively involved with organizations like the American Academy of Orthopedic Surgeons (AAOS), Dr. Gough's his drive for excellence is visible outside his direct practice. Serving as Vice President of the Orthopedic Surgery Interest Group, he also keeps active memberships with the American Medical Association and American College of Physicians. Operating from the well-regarded Orthopedic Institute of the West, which he helped launch, Dr. Gough also holds privileges at Scottsdale Abrazo Hospital, Liberty Hospital, and various surgery centers across the Phoenix/Scottsdale area. Fueled by his passion for innovative surgical techniques, he orchestrates the development of a robotic hip and knee replacement center of excellence while also mentoring surgeons worldwide.
Apart from his career achievements, Dr. Gough is steadfast in his commitment to community service, actively volunteering with charities like the Magis Clinic, Madonna School, Habitat for Humanity, and Sienna St. Francis Clinic.
Essentially, his ongoing consultancy with Zimmer Biomet underlines his dedication to pushing forward the boundaries of orthopedic surgical care.
Planet TV Studios Profile: Planet TV Studios produces cutting-edge, real-life television series featuring insightful updates on crucial business, medical, and socially responsible topics.
To learn more about Gough Surgical, PLLC, please check out https://goughmd.com.
For comprehensive details about the series, please go to https://planettvstudios.com / https://planettvstudios.com/backstage/ or contact Christian Alain at 888-210-4292 x100 or email christian@planettvstudios.com.
Gough Surgical Adult Hip & Knee: Commanding the Next Era of Orthopedic Care
Amid the landscape of skeletal surgery, precision, know-how, and modernization come together at Gough Surgical Adult Hip & Knee, a respected center specifically catering to adult hip and knee prosthetic procedures.
Under the expert leadership of Dr. James Gough, this specialized institution has garnered acclaim for revolutionizing patient experiences by rejuvenating mobility, alleviating pain, and remarkably uplifting life standards for many individuals.
Setting New Standards in Orthopedic Surgery
Skeletal procedures, notably focused on hips and knees, constitute the most prevalent operations conducted internationally.
Still, the success and patient satisfaction rates show substantial variation resulting from surgical expertise, facility quality, and the surgeon's approach.
Gough Surgical differentiates itself by specializing only in adult hip and knee interventions, fostering concentrated know-how rare in the general industry.
Dr. James Gough, acknowledged for his precise surgical methods and patient-oriented service, has focused his career on honing these sophisticated surgeries.
His clinic, Gough Surgical Adult Hip & Knee, ideally positioned to assist patients across different locales, has come to represent excellent clinical results, prompt recoveries, and improved patient experience.
Excellence Founded on Expertise
Why dedicate practice solely to adult hip and knee replacements?
In the view of Dr. Gough, focusing on a niche yields unrivaled skill.
"By focusing solely on adult hip and knee replacements, we've developed an unparalleled level of proficiency," affirms Dr. Gough.
This specialized knowledge yields reduced incident rates, lower surgical hazards, and boosted patient results.
State-of-the-Art Surgical Approaches and Tools
Gough Surgical Adult Hip & Knee routinely adopts leading-edge technology to sharpen surgical precision and patient outcomes.
One of the key highlights of the practice entails employing innovative robotic surgery technology.
These innovative technologies facilitate remarkable precision, bringing about accurate prosthetic positioning personalized to the patient's anatomical needs.
"Robotic assistance doesn't replace the surgeon's expertise—it enhances it," asserts Dr. Gough.
Patient-Oriented Care: More Than Just Surgery
At Gough Surgical, the approach to patient care surpasses the confines of the operating room.
From the initial meeting through in-depth post-operative assessments, patients receive personalized, attentive care every step of the way.
This comprehensive strategy ensures effective physical rehabilitation and boosts mental comfort and certainty throughout the healing journey.
Dr. Gough underscores, "Acknowledging every patient's individual needs, insecurities, and goals is indispensable." Customized care markedly affects recuperation speeds and overall patient approval.
All-Encompassing Pre- and Post-Surgical Assistance
Gough Surgical’s devotion to extensive care shows itself via its in-depth preoperative protocols and comprehensive postoperative check-ups.
Dedicated preoperative learning classes, specialized patient workshops, and individualized advisory sessions prepare patients physically and mentally, mitigating worry and nurturing informed selections.
Post-surgery, the center’s well-defined recuperation procedures and tailor-made physical rehabilitation plans yield quicker, more consistent recoveries.
Clients favor the transparent instruction, periodic progress reviews, and uncomplicated access to seasoned advice, markedly elevating their rehabilitative outcomes.
Cutting-Edge Approaches to Challenging Conditions
Gough Surgical Adult Hip & Knee thrives in handling complex scenarios that may overwhelm other centers.
Ranging from elaborate joint reconstruction surgeries to tackling advanced arthritis challenges, the facility presents inventive strategies through state-of-the-art operative techniques, low-impact approaches, and custom-designed implant solutions.
These these tailored treatments typically produce rapid recovery, decreased postoperative aches, and rejuvenated movement, allowing individuals to return to vibrant, pain-free living with speed.
An Enduring Record of Patient Approval
The patient stories attest to the remarkable improvements achieved through its treatments.
Individuals often recount regained autonomy, marked decreases in pain, and improved life quality post-treatment.
"Walking without pain was something I never imagined possible again," says Mary Thompson, a patient who underwent a total knee replacement at Gough Surgical.
"Dr. Gough and his team didn't just restore my knee—they gave me my life back," continues Mary Thompson.
Advancements in Research and Education
Beyond medical proficiency, Gough Surgical Adult Hip & Knee actively fuels advancements in orthopedic care with continuous research and training.
Dr. Gough frequently contributes to clinical research, delivering key data that improves orthopedic practices and patient outcomes.
Additionally, the center facilitates routine educational sessions and collaborative workshops, supporting professional growth among healthcare providers and progressively lifting industry norms.
A Future-Oriented Method in Orthopedics
As the domain of orthopedic care advances, Gough Surgical remains at the forefront of innovation, constantly integrating new technologies and methodologies.
The practice’s drive for continuous progress ensures the delivery of cutting-edge and effective treatments.
"{Our goal is to redefine what's possible in orthopedic surgery continually," states Dr. Gough.
"Innovation and patient care must evolve hand-in-hand," declares Dr. Gough.
Conclusion: Pioneering the Future of Hip & Knee Care
Gough Surgical Adult Hip & Knee stands as a beacon of excellence in orthopedic care, blending advanced surgical innovation, unmatched specialization, and compassionate patient engagement.
By steadily advancing beyond conventional boundaries, Dr. James Gough and his dedicated team not only reinstate joint function—they dramatically enhance lives.
In the expedition toward effortless motion and revitalized well-being, Gough Surgical Adult Hip & Knee is not just reshaping orthopedics—it is crafting the future benchmarks for medical care.
Minimally Invasive & Muscle-Conserving Surgical Methods: Reshaping Contemporary Medicine
In recent decades, surgical innovation has recast patient care, promising minimal trauma, faster recovery, and elevated outcomes.
Among these advancements, micro-invasive and muscle-sparing surgical methods have come forth as transformative techniques.
These strategies have not only transformed the operating room, but also revolutionized the patient experience.
This article reviews the evolution, techniques, benefits, challenges, and future directions of minimally disruptive and muscle-guarding methods, harnessing expert insights, clinical studies, and real-world applications.
A Modern Epoch in Surgery: The Increase of Minimally Invasive Approaches
The modern operating room is poles apart from the large incisions and extended hospital stays that marked surgical procedures a century ago.
Surgeons today are steadily adopting techniques that minimize tissue disruption and preserve the natural anatomy of the body.
Essential to these progressions are micro-invasive and muscle-sparing procedures.
Micro-invasive surgery means methods that rely on small incisions, custom-made instruments, and crystal-clear imaging to access and treat internal issues with minimal interference to nearby tissues.
In contrast, muscle-conserving surgery is dedicated to upholding the wholeness of muscle tissue during operations once demanding significant muscle dissection.
Both methods are part of a broader movement toward reducing patient morbidity, pain, and recovery time.
Historical Reflections: From Conventional Open Surgery to Tissue-Sparing Methods
Historically, the approach to surgery was defined by need and accessible technology.
Before the advent of modern imaging and instrumentation, operative physicians routinely resorted to broad, open incisions to ensure clear visibility and access the operative field.
Even though these methods were life-preserving, they typically imposed substantial postoperative pain, extended recuperation, and increased the likelihood of complications like infections or persistent muscle debility.
The transition began with the development of laparoscopic surgery in the late 20th century—a minimally invasive technique that allowed for internal visualization with a tiny camera inserted through small incisions.
As technology advanced, surgeons began to appreciate that preserving muscle integrity during procedures could offer even greater benefits.
Muscle-sparing techniques, initially developed in orthopedics and cardiovascular surgery, soon found applications in abdominal, gynecological, and oncological procedures, among others.
Dr. Eleanor Matthews , an innovator in minimally invasive procedures at a leading teaching hospital, remembers: “We realized that every incision we made, every muscle we cut, had a lasting impact on our patients. The drive to improve quality of life post-surgery has pushed us to continually refine our methods.”
This transition toward more patient-friendly procedures illustrates both a technical triumph and a fundamental shift in surgical philosophy.
The Science Behind the Techniques
Minimally Invasive Surgery: Accuracy via Technology
The underlying tenet of micro-invasive surgery is precise execution.
Surgeons use an array of high-tech tools—from endoscopes and robotic-assisted devices to specialized microscopes—to navigate the human body through minuscule openings.
These instruments provide enhanced magnification and illumination, enabling the precise identification and treatment of the target area without extensive tissue damage.
One of the most significant innovations has been the integration of robotic-assisted surgical systems.
These systems provide surgeons with unparalleled steadiness and accuracy, countering natural hand tremors and converting nuanced movements into finely have a peek at these guys controlled actions.
In procedures such as prostatectomies and cardiac surgeries, this precision translates directly into improved patient outcomes.
Cardiothoracic Surgery: Minimizing Cardiac Trauma
Cardiothoracic operations have considerably gained from micro-invasive approaches.
Interventions including valve repair and CABG have traditionally involved wide incisions and significant muscle tissue dissection.
Today, surgeons increasingly employ minimally invasive techniques that use small incisions and specialized instruments to access the heart and surrounding structures.
The adoption of robotic-assisted systems in cardiothoracic surgery has further refined these procedures.
Frequently, these robotic platforms provide the fine precision necessary for delicate maneuvers on the beating heart, lowering complication risks and facilitating quicker recovery.
Research documented in the Annals of Thoracic Surgery indicated that patients treated with minimally invasive valve repairs showed lower incidences of postoperative atrial fibrillation and experienced reduced hospital stays compared to those treated with standard surgery.
General and Gynecologic Treatments: Enhancing Patient Outcomes.
In the realm of general and gynecologic surgery, micro-invasive techniques have transformed procedures such as gallbladder removals, hernia repairs, and hysterectomies.
Transitioning to smaller incisions with muscle preservation minimizes both visible scars and postoperative discomfort, while also reducing complication risks.
For example, laparoscopic cholecystectomy—the removal of the gallbladder via small incisions—has emerged as the global standard of care.
Patients benefit from shorter recovery times and the ability to resume normal activities almost immediately after the procedure.
In gynecology, muscle-sparing techniques have been instrumental in improving outcomes for women undergoing complex procedures such as myomectomies or pelvic floor repairs.
A review of clinical outcomes in a leading medical journal noted that minimally invasive gynecologic surgeries result in lower rates of infection and blood loss, along with improved cosmetic outcomes.
These improvements serve to boost patient satisfaction as well as to yield better overall health outcomes.
Weighing the Benefits and Challenges.
Benefits That Extend Beyond the Operating Room.
Advantages inherent in micro-invasive and muscle-sparing methods go well beyond the procedural technicalities.
For patients, the benefits are tangible and life-changing.
The reduction in pain, scarring, and recovery time directly translates into a better quality of life.
In many cases, patients can return to work and resume daily activities within days rather than weeks, a critical factor in an increasingly fast-paced world.
From a comprehensive healthcare viewpoint, such techniques reduce overall hospital costs by minimizing both the length of stay and the postoperative care needed.
Additionally, fewer complications mean fewer readmissions, which is a significant consideration for healthcare providers and insurers alike.
The psychological benefits should not be underestimated.
Being aware that a procedure is minimally invasive reassures patients and alleviates preoperative anxiety.
This factor is vital for patients scheduled for major surgeries, as a calm, optimistic outlook can enhance overall recovery and outcomes.
Challenges and Limitations: A Realistic Perspective.
Despite the numerous advantages, micro-invasive and muscle-sparing techniques are not without challenges.
One significant limitation is the steep learning curve associated with these advanced methods.
Surgeons must undergo rigorous training and gain substantial experience before they can perform these procedures with the same level of proficiency as traditional surgeries.
High initial costs for advanced technology and training may restrict accessibility in resource-constrained areas.
Also, these approaches are not universally applicable to all patients.
For cases marked by extensive pathology or complex anatomy, the traditional open approach may be preferable and safer.
Surgeons are required to carefully analyze every situation, comparing the benefits of minimally invasive approaches with the patient’s individual circumstances.
Moreover, technical limitations are another important factor.
Even with modern, state-of-the-art tools, limitations in the operative field or unforeseen complications can occur, which may require a switch to an open procedure.
Although such cases are uncommon, they underscore the necessity of a flexible surgical team capable of adapting to unforeseen challenges.
Expert Insights and Patient Perspectives
Echoes from the Frontline
Dr. Michael Andersen, a celebrated surgeon boasting over 25 years in minimally invasive techniques, underscores the significance of tailored patient care
“Every individual is one-of-a-kind, and while micro-invasive and muscle-sparing techniques offer significant advantages, the essential task is to tailor the intervention to the patient’s specific needs and overall wellness,” he explains.
His insights underscore a fundamental tenet of modern medicine: technology must serve the patient, not dictate the treatment plan.
Likewise, individuals who have experienced these procedures frequently describe the life-changing impact on their overall well-being.
Maria Lopez, a 54-year-old patient who recently received a muscle-sparing breast reconstruction, reflects on her experience.
“I was prepared for a long, painful recovery. Instead, I was up and moving within days. It felt as if I had been given a second chance at life,” she observes.
Such testimonials, while anecdotal, are supported by robust clinical data that points to improved outcomes with these techniques.
Forging a Trustworthy Surgical Network.
The growing popularity of micro-invasive and muscle-sparing methods is fostering a broader cultural shift in healthcare.
Surgeons, hospital systems, and training initiatives are working jointly to share best practices, standardize protocols, and back ongoing research.
Conferences and symposiums dedicated to minimally invasive techniques are now a regular feature in the medical community, providing a forum for experts to discuss innovations, challenges, and future trends.
Such integrative collaboration is fundamental to surmounting the issues associated with these advanced surgical methods.
By pooling expertise and resources, the medical community is better positioned to refine surgical methods, reduce complications, and ensure that the benefits of these techniques are accessible to a wider population.
The Future of Surgery: Trends and Innovations.
Integrating AI-Based and Robotic Technologies.
While contemporary micro-invasive and muscle-preserving techniques have had a major impact, the future is anticipated to bring even more groundbreaking changes.
The integration of artificial intelligence (AI) and machine learning into surgical systems is poised to further enhance precision and efficiency.
These technologies can analyze vast amounts of data in real time, offering surgeons predictive insights that may improve decision-making during complex procedures.
For example, AI-powered imaging systems are being developed to automatically highlight critical anatomical structures, reducing the risk of inadvertent injury.
Robotic platforms are also evolving, with next-generation systems offering even finer control and enhanced haptic feedback, which allows surgeons to "feel" the tissue they are operating on—a feature that traditional laparoscopic instruments lack.
Extending the Frontiers of Minimally Invasive Procedures.
Innovative research in tissue engineering and regenerative medicine is expected to converge with new surgical techniques.
Scientists are seeking approaches to curtail tissue injury and promote expedited, natural healing.
This includes the use of bioengineered scaffolds that can support tissue regeneration and reduce scar formation after surgery.
Moreover, as imaging and sensor technology continue to improve, surgeons may be able to perform procedures that are even less invasive than those currently available.
Emerging technologies, including nanorobots and micro-implantable devices, hold the promise of enabling targeted cellular therapy and diagnostics, thus heralding a new age of personalized medicine.
A Universal Outlook: Linking the Disparities in Surgical Services
Although groundbreaking technological advancements are redefining surgery in developed nations, substantial imbalances in access to modern surgical care remain globally
Narrowing the divide will depend on joint strategies from governments, philanthropic bodies, and the global health community
Instructional programs, tech-transfer initiatives, and cooperative research projects are vital to ensure that patients around the world enjoy the advancements in micro-invasive and muscle-sparing procedures
Worldwide collaborations are beginning to show promising results
Medical centers in well-funded nations are joining forces with clinics in emerging markets to supply training and technical support for minimally invasive procedures
These alliances not only enhance clinical results but also cultivate a fairer and more balanced worldwide healthcare framework
Navigating Tomorrow: Difficulties and Potential Opportunities
The march toward comprehensive use of cutting-edge micro-invasive and muscle-preserving surgery is impeded by a range of challenges
The monetary commitment for state-of-the-art apparatus, coupled with the demand for expert training, can be substantial
Yet, the long-term benefits, including enhanced patient results and significant cost savings in healthcare, imply that these challenges are surmountable
Government authorities and healthcare administrators are beginning to see that allocating funds for state-of-the-art surgical innovations can generate considerable benefits
Shorter periods of hospitalization, fewer clinical complications, and a swift return to work enhance patients’ quality of life while reinforcing a more resilient and efficient health system
As a result, both public and private stakeholders are directing greater resources toward the evolution and propagation of these advanced techniques
Also, the cultural landscape among surgeons is undergoing a notable transformation
A commitment to ongoing academic growth, interdepartmental collaboration, and evidence-supported approaches is establishing a culture where innovation is both embraced and anticipated.
This change in cultural dynamics is expected to hasten the uptake of cutting-edge techniques and futuristic technologies, ultimately improving patient outcomes universally.
Summary: A Revolutionary Shift in Delivering Patient-Centered Surgical Services.
The advancement of micro-invasive and muscle-preserving techniques marks a revolutionary turning point in how surgical care is administered.
These procedures have set new standards in the OR by focusing on exacting precision, reducing surgical trauma, and preserving muscle, ultimately leading to superior patient results.
From the formative stages of laparoscopic surgery to today’s blend of robotics and AI, the pathway has been paved with constant innovation and a resolute drive for excellence.
For patients, these techniques offer the promise of diminished pain, accelerated recovery, and an elevated quality of life.
For surgeons and healthcare providers, the challenge is to master these innovative techniques, invest in cutting-edge technology, and cultivate a culture of constant advancement.
As research deepens and technology continues to advance, the likelihood of new innovations in micro-invasive and muscle-preserving surgery is substantial.
Future surgical paradigms will focus on patient-centric care, with devices and procedures designed to improve, not impair, the body’s natural capabilities.
Peering into the future, the integration of state-of-the-art imaging, robotic technology, and regenerative therapies promises to open new horizons in patient-focused care.
The ever-progressing landscape of surgical practices is a tribute to the healthcare community’s enduring commitment to innovation, safety, and enhanced patient outcomes.
In today’s era of customized healthcare, micro-invasive and muscle-sparing techniques are not merely technical upgrades; they stand as a testament to the promise of a less intrusive and more patient-friendly future.
As we progress, every advancement brings us closer to a world where surgery no longer heralds pain and prolonged recuperation, but instead offers a pathway to restored health and vibrancy.
Further Documentation and References.
Clinical Studies and Reviews: Extensive clinical investigations documented in journals like the Journal of Minimally Invasive Surgery, Annals of Thoracic Surgery, and the Journal of Surgical Education present solid data supporting the improved outcomes associated with these methods.
Expert Interviews: Testimonies from prominent surgeons such as Dr. Eleanor Matthews, Dr. Luis Hernandez, and Dr. Michael Andersen offer valuable insights into both the advantages and the practical challenges of these techniques.
Technological Innovations: Breakthroughs in robotic-assisted surgery and augmented reality are featured in current scientific literature and serve as key topics at worldwide surgical conferences.
By focusing on precision, reducing operative trauma, and preserving muscle function, micro-invasive and muscle-sparing methods have inaugurated a new era of patient-centered care, significantly boosting both clinical outcomes and the patient experience.
As innovation in technology accelerates and healthcare providers worldwide adopt these breakthroughs, the future of surgery promises even more significant advantages for patient care.
In this fast-evolving arena, the relentless pursuit of ongoing enhancement is the definitive indicator of progress—a commitment that will transform surgical care for future generations.
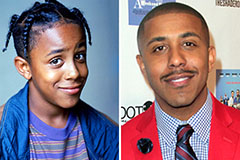 Marques Houston Then & Now!
Marques Houston Then & Now! Elin Nordegren Then & Now!
Elin Nordegren Then & Now! The Olsen Twins Then & Now!
The Olsen Twins Then & Now! Sarah Michelle Gellar Then & Now!
Sarah Michelle Gellar Then & Now! Ryan Phillippe Then & Now!
Ryan Phillippe Then & Now!